Contact Your Insurance Company
Contact your insurance company to verify your current benefits and if Yellowstone Surgery is considered an In-Network Facility. Also determine your benefits and to find out if your insurance company requires a pre-authorization.
Pre-Authorization
- Pre-authorization for surgical procedures is done by your physician’s office.
- Pre-authorization for pain procedures is done by Yellowstone Surgery Center.
- Pre-authorization does not guarantee payment from your insurance.
- Your insurance company may deny payment if pre-authorization is not completed.
Don’t Have Insurance?
If you do not have insurance, prior to your procedure, you will need to contact Yellowstone Surgery Center to speak with a Patient Representative to discuss payment options.
Insurance Billing
As a courtesy to you, we will file a claim with your primary insurance company. Please make sure to provide us with the necessary information. In most cases, payment is sent directly from your insurer to us within 4-6 weeks. We will then bill your secondary insurance company should you have one and if you have provided us with that information. If your insurance company or companies have not met their obligation within 6 weeks, we advise that you contact them directly to verify the status of your claim and the date on which payment is expected to be made.
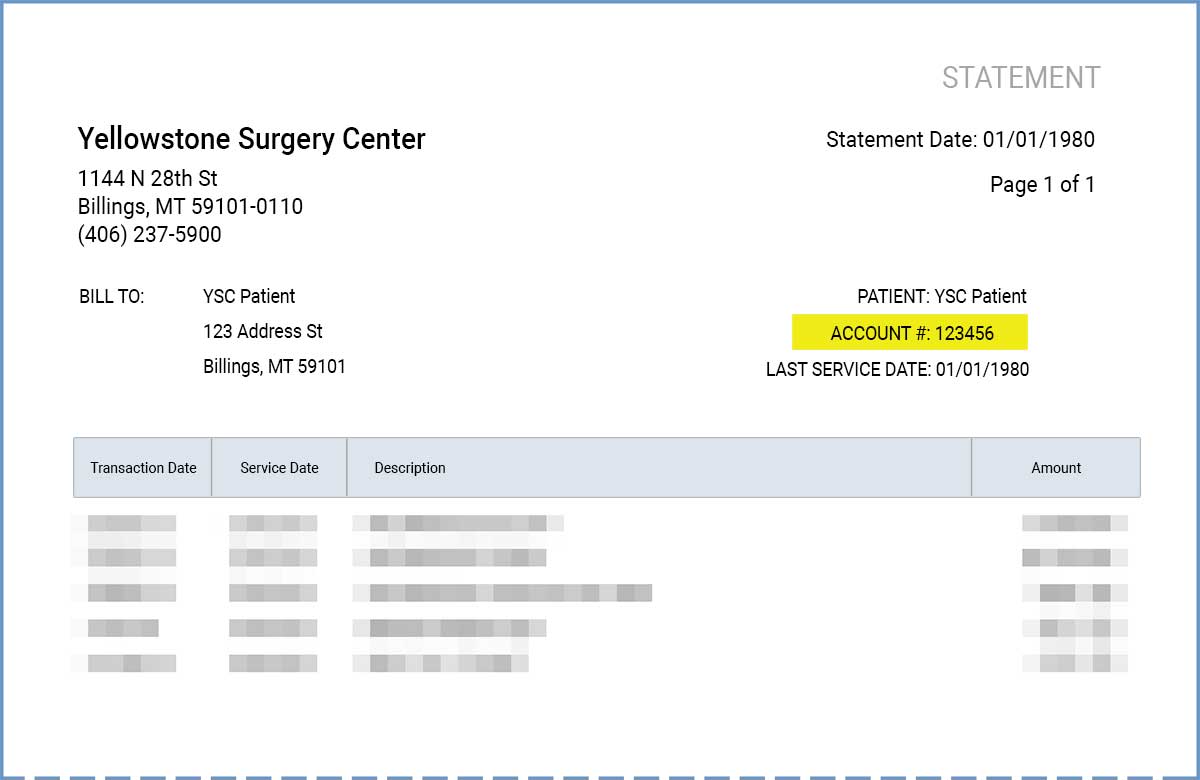
Once your insurance company(s) have responded, you will receive a statement from our office. It will detail your date(s) of service, insurance payments or adjustments and any remaining balance for which you remain responsible.
If you have a Cost-Sharing Program, Yellowstone Surgery Center will provide you with an itemized bill to submit to the program. Monthly payments will be required until the Cost Sharing program remits payment.
You will not receive a bill from Yellowstone Surgery Center until your insurance has processed your claim.
Medicare
Yellowstone Surgery Center does accept assignment on Medicare claims. We will bill Medicare and, when we receive payment, they will instruct us on how much to discount and how much we are to bill you or your secondary insurance. If you have secondary insurance, we will bill it at this time. Any balance remaining after we receive their payment will be your responsibility.
Additional Charges
Payment arrangements are made prior to surgery; however, additional fees may be incurred due to unforeseen circumstances. Each case is different and, if necessary for your health and safety, your physician may order additional supplies or conduct different or additional procedures than those originally scheduled. Although these fees were not included in your original estimate, you will be billed for them.
Remaining Balance
If you have a balance after your insurance pays, the balance will need to be paid off in four to six months with regular monthly payments. It is important to contact our Billing Department should you have difficulty paying your balance off in this amount of time. There are options that may be available to you.
 Patient Responsibility
Patient Responsibility